The use of PBS for autistic people has generated a lot of debate. Many autistic people say that, when used as a derivative of ABA, PBS is damaging and traumatic. On the other hand, some family members believe it has been a lifeline for their loved one.
As part of the first in the series, ‘Rightful Lives Investigates’, we want to look at people’s experiences and gather views. We’d really like it if people could send us their stories in any form with which they feel comfortable. For example, this could be written down, a recording or a video.
We will initially publish these here on our blog. We are designing a new website so eventually they will be transferred to that.
To start us off, Alexis Quinn has prepared a video of her experience of PBS. Alexis is putting her own experience forward and appreciates that everyone’s experience is unique. Click on the You Tube link to watch her video.
PBS & ABA part 2
Following our opening blog by Alexis Quinn on the topic of PBS, we are now publishing the views of another contributor. Behaviours mentioned have been changed to protect privacy and the author wishes to remain anonymous. We welcome other contributions to keep this debate going.
“I wanted to contribute to the “Rightful Lives Investigates” on PBS as someone who values the perceptions of autistics lived experience, as the sibling of an autistic, as the mother of an autistic, but also as someone who has had an experience from the “other side of the fence”.
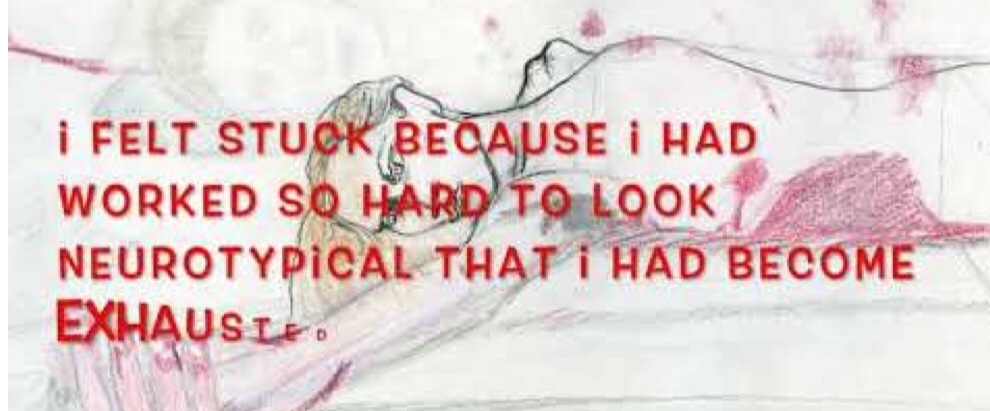
A few years ago i was a Support Coordinator, managing a team of staff, coordinating care packages and working with family members. I had a background working in residential, supported living and psychiatric hospitals. I have always, despite being female always been delegated to posts that support people who are “complex” or have “challenging behaviour”. In my experience what this means is people who do not communicate verbally and who have co-morbid physical, developmental or mental health issues. I have always been uncomfortable with physical restraint. I have experienced it myself in my youth and resented training which focused on physical restraint such as PMVA. When i was trained in PBS it finally felt like a format I could work with. As a team leader my staff were not taught how to restrain the people we supported which felt like a massive step forward. They were taught that standing blocking a door was restrictive, they learnt locking the back door was restrictive, they learnt about least restrictive practice and it helped. Some of the people I worked with were being restricted by their family members, they were hurting themselves trying to communicate their needs, their physical, emotional and sensory needs were not being met. PBS gave me a format by which I could investigate more thoroughly, find and communicate the reasons behind behaviour and outline what the staff team were expected to do in writing. This meant that I was given time to identify and work directly with the people my team supported at the times they most needed support (rather than on a rota system), i had staff who were actively observing everything and documenting it rather than receiving a quick note that someone had self harmed. It meant that I could tell a parent ; “when you do x your family member hurts themself, therefore I am firmly asking you to consider whether you need to do that” and take appropriate action to educate them and explain which laws protected their right not to be restricted. It meant that I could identify that perhaps someone is flapping their arms because they need to get away from noise and they need physical movement to regulate themselves and put it in writing to remind that person that they can go outside to get away from the noise and use a swing. That perhaps the person banging their head on the floor with a blanket over their head has a headache and may feel better if we offer paracetamol and some quiet time in a dark space. The plans I wrote explored the needs of the people I was paid to support- i can say with a fair amount of certainty that no part of their plan tried to make them neurotypical, if anything it provided more evidence that we needed to provide more sensory input, the plans gave me evidence that I could use to agree an increase in commissioned support hours.
Basically, when I completed my qualification in care management I educated myself on PBS, where it came from and why some parts of it’s history such as ABA were extremely negative. The only part of ABA that we were required to use was a documentation of what happened before, during and after an incident. This meant that i could see what could have upset the person and what had or hadn’t worked. It also kept my staff team accountable for their actions. The main thing that could have been different from the experiences of PBS that I have heard autistic people talk negatively about is the aims. My aims were always based on communication improvement (including sending members of staff on courses, teaching them on shift and making resources available), and environment improvement (including reducing triggers and providing sensory equipment that was accessible at all times). We didn’t target autistic behaviours, we targeted behaviours that were communicating an unmet need. It was never about changing a person, it was about putting right a system of neglect and misunderstanding. I feel that behaviour has a massive place in communication and that we need to be listening to and understanding those behaviours. Another person I knew would say (phrase changed for privacy) that they were going to hit the wall whenever they were in public places. As a result their activities in the community were really restricted. The first time this person said this to me we were in a busy shopping centre, in short I basically said something along the lines of “you could do that, we would probably be asked to leave and may not be able to come back again, or if it’s too much to wait for our shopping today we could just get a taxi home and come back tomorrow?”… they chose to get in the taxi, we went home and i wrote it in a behavioural support plan that if they started talking about hitting walls to give the option to leave immediately and schedule an alternative time to complete the task. The person learnt that people would listen to them when things were too much. There were no rewards or punishments, but natural consequences of having needs met and increased access to community activities could be argued to be a reinforcer. The staff team learnt that they could provide options instead of restricting a person.”